ASPEN: Capsular Contracture
Sometimes, no matter how skilled a patient’s plastic surgeon is, complications arise during or after surgery. This is the case because everyone’s body is different. The composition of connective tissue varies widely from one patient to another, for instance, and this means that each patient’s healing process is entirely unique. This is why some people tend to develop thick scar tissue (known as keloid scar tissue) after any kind of penetrating skin injury, while others can sustain deep cuts and develop only subtle scarring that fades over time. Another good example of this difference is the way some women will develop severe stretch marks during pregnancy no matter what they do to prevent them, whereas other women emerge from pregnancy nearly stretch mark-free. Additionally, everyone’s immune system responds differently to stimuli. Just like some people have bodies that reject medical implants (despite the fact that these are designed to be completely biocompatible), some patients’ immune systems react poorly to implants inserted for cosmetic reasons.
Of course, complications during plastic surgery are now very rare, both because of advances in surgical techniques and because we’ve gotten better at predicting which patients are likely to experience surgical complications. Patients who are prone to developing thick scar tissue may be advised to avoid having plastic surgery, or their surgeon will use special surgical techniques that allow incisions to be placed remotely (e.g., inserting breast implants through an incision in the underarm) in order to keep scarring largely out of sight. Patients who have compromised immune systems or autoimmune diseases are often advised to forego surgery and choose less invasive forms of cosmetic enhancement. Likewise, there are a number of procedures that can be used after surgery, such as ASPEN, in order to treat complications and improve the patient’s appearance. One of the most common areas where ASPEN is used is in the treatment of capsular contracture after breast augmentation surgery.
What is Capsular Contracture?
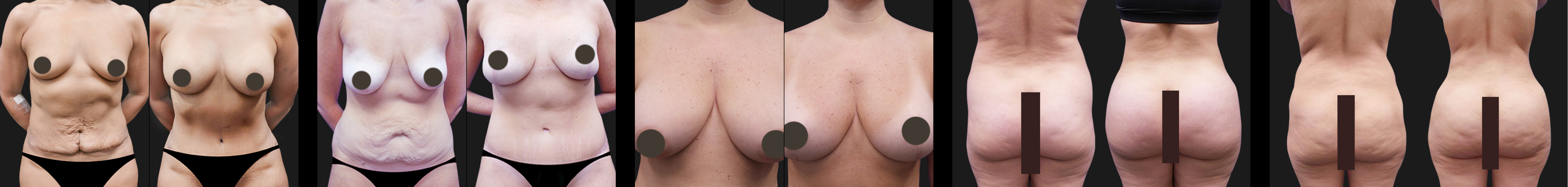
The formation of a “capsule” of scar tissue around any kind of implant (medical or cosmetic) is a normal part of the healing process. The body automatically reacts to any foreign object it detects within it and attempts to isolate said object by creating a barrier of scar tissue around it. In the case of breast implants, this is usually a good thing—the capsule helps to keep the breast implants in place, preventing slippage. In some patients, however, this capsule of scar tissue becomes unusually hard and starts to contract around the implant. This can lead to both aesthetic problems and, in extreme cases, pain in the breasts. Research shows that about one in six breast augmentation patients experience some degree of capsular contracture, though not all cases present with obvious symptoms. The severity of capsular contracture is rated using a grading system:
Grade 1: Grade one capsular contracture is asymptomatic. The formation of scar tissue around the implant does not interfere with the size, shape, or texture of the breasts. The breasts look natural and remain soft to the touch.
Grade 2: Grade two capsular contracture usually presents itself with only minor cosmetic symptoms. The breasts will usually appear normal in shape but feel somewhat firm to the touch.
Grade 3: Grade three capsular contracture presents itself with obvious cosmetic symptoms. The breasts will be firm to the touch and appear abnormal, e.g., they will be overly round, hard-looking, and the nipples may be misshapen. However, this grade of capsular contraction often doesn’t cause much (if any) pain.
Grade 4: Like grade three capsular contracture, grade four capsular contracture causes the breasts to become hard and misshapen. Patients with grade four capsular contracture also experience breast soreness; their breasts will often be tender and painful to the touch.
Generally, capsular contracture occurs during the healing process. About 75% of all capsular contractures will occur within two years of the patient’s implants being placed. Sometimes capsular contractures occur many years after breast augmentation surgery, but this is the exception rather than the rule. If this does occur, the patient’s breast implants should be checked for ruptures. Ruptured implants are the most common cause of late-onset capsular contraction.
What Causes Capsular Contracture?
Clinicians have a number of theories on what causes capsular contracture, and it’s likely that the exact causes of this condition vary from patient to patient. As a breast augmentation patient, it’s important to understand that this condition is not caused by breast implants being in any way toxic or dangerous. Saline implants contain only saline solution, which can be safely reabsorbed by the body with no ill effects, and silicone gel implants are made of medically inert silicone. Indeed, capsular contracture can happen after any kind of medical implant is inserted into the body; the condition is not unique to breast augmentation surgery. Capsular contracture is just particularly troubling when it occurs after breast augmentation because it often alters the appearance of the breasts, thereby jeopardizing the aesthetic improvements that the patient had surgery to create. Capsular contracture is not usually dangerous to the patient’s health unless her implants have ruptured (in the case of gel implants, rupture can sometimes lead to infection).
Researchers believe genetics play a role in who develops capsular contraction and who does not. If you have a family history of autoimmune disease or you have relatives who frequently develop thick scar tissue after injury (or who have had difficulties with medical implants), then you may have a slightly heightened risk of developing this condition. However, it’s impossible to accurately predict who will develop a “random” case of capsular contracture (i.e., one that is not caused by any identifiable external factors) and who will not. Because capsular contracture is highly treatable, you shouldn’t let a fear of developing this condition hold you back from getting breast augmentation surgery.
Sometimes, capsular contracture is caused by something other than the patient’s own body reacting poorly to the presence of breast implants. In addition to implant ruptures, it is now believed that something called “biofilm” often leads to the development of this condition. Biofilm is a thin layer of bacteria that develops around implants after a type of bacteria (often staph bacteria) is introduced to the breast cavity during surgery. This bacterium causes a kind of chronic, low-grade infection that may not produce noticeable symptoms (such as fever or severe fatigue). However, as the body combats this infection, it produces more and more fibrous scar tissue, eventually leading to capsular contracture. The biofilm theory of capsular contracture was given credence by a recent study conducted on pigs who were implanted with medical-grade silicone implants. This study showed that there was a significant increase in the likelihood of capsular contracture in those pigs who had staph bacteria on their skin at the time of implant placement. It’s important to note that staph contamination during breast augmentation surgery does not necessarily result from an unhygienic working environment. Some people are natural carriers of staph bacteria; it’s always present on their skin and usually causes no symptoms. Only when these individuals have their skin penetrated does this bacterium have a chance to cause any serious issues. While ensuring a clean working environment can certainly help to lower the risk of staph contamination, it’s not always possible to eliminate 100% of the bacteria that’s present.
Other rare complications of breast augmentation surgery, such as hematomas and seromas (blood clots that sometimes form after invasive surgery), are also believed to increase the risk of capsular contracture. Some researchers believe these blood clots increase the likelihood of capsular contracture by providing a rich supply of nutrients (in the form of blood) for bacteria, thereby encouraging the growth of biofilm.
How Can Capsular Contracture be Prevented?
While it’s impossible to prevent capsular contracture from occurring in every patient, there are several ways to lower a patient’s risk of developing this condition. To that end, plastic surgeons now employ a number of different preventative strategies, as outlined below:
- Thorough patient screening – Patients are screened for health conditions that might increase their risk of complications like hematomas. Patients are also required to give up smoking, as smoking makes hematoma formation more likely and generally impairs the healing process.
- Using the correct size of implant for the patient – Placing a large implant in a patient with insufficient natural breast tissue to cover said implant increases the risk of capsular contracture. If a patient with small breasts wants to increase her cup size significantly, it’s better to do so in stages, e.g., start with a mid-sized implant and give the skin time to stretch before placing a larger one.
- Minimal implant handling – The more an implant is handled prior to being inserted into the patient’s breast, the more likely bacterial contamination becomes. As such, surgeons strictly limit how much they touch any implant before placing it in the patient’s body. Board certified plastic surgeons also work in a sterile hospital facility, just like medical surgeons do.
- The use of textured gel implants – Using gel implants with a textured surface, rather than a smooth surface, has been shown to reduce the likelihood of capsular contraction. It is thought that the textured surface of the implant makes it more difficult for thick scar tissue to develop around the implant. However, textured implants are not right for every patient, as in some cases their edges may be more detectable. They are usually most suitable for use when the implants are being placed below the chest muscles.
- The use of “under the muscle” placement – Placing implants under the chest muscles can significantly lower the risk of capsular contracture. Partial under the muscle implant placement results in an 8-12% lifetime risk of capsular contracture, as opposed to a 12-18% lifetime risk of capsular contracture with over the muscle implant placement. Furthermore, implants that are placed completely under the muscle are associated with just a 4-8% lifetime risk of capsular contracture.
- Massage – Gently massaging the breasts while they heal from breast augmentation surgery may help to prevent capsular contracture by encouraging the breast tissue to remain pliable. However, this method has not been proven effective by any major studies. You should never disturb the tissue of your breasts while they are healing from surgery without first getting permission from your surgeon. Otherwise, you may damage the tissue and make capsular contracture more likely.
How Does ASPEN Treat and Reverse Capsular Contracture?
In the past, the treatment options available for breast augmentation patients with capsular contracture left much to be desired. Revision surgery was often required—a lengthy, costly, and uncomfortable solution. During this process, the patient’s implants were removed, she was treated with antibiotics, and eventually (once the infection had subsided), she could choose to have breast implants inserted again. However, because this surgical approach makes the body vulnerable to a second bacterial invasion, many of these patients experienced repeated incidences of capsular contracture.
ASPEN Multi-Energy Therapy is different: It’s completely noninvasive, so it doesn’t cause the patient pain or inconvenience, nor does it increase her risk of developing capsular contracture again in the future. During ASPEN therapy, a special device (the ASPEN harmonizer) is applied to the patient’s breast tissue, without any incisions being made. The ASPEN harmonizer delivers precisely controlled ultrasound waves to the patient’s tissue, encouraging the growth of healthy collagen. This increases elasticity within the breast capsule around the implant, making the breasts feel soft and pliable again. Furthermore, the ultrasound waves used during ASPEN therapy have been shown to increase the effectiveness of antibiotics in combating biofilm. ASPEN therapy is usually administered over two to three weeks in combination with antibiotic therapy to target the root cause of capsular contracture. The ASPEN method has been shown to be effective for grade two and grade three cases of capsular contracture. Grade four cases may require more aggressive surgical intervention.
If you’re a good candidate for ASPEN therapy, this completely safe, pain-free procedure can treat and reverse capsular contracture. Feel free to contact us to learn more about this procedure.

 Sometimes, no matter how skilled a patient’s plastic surgeon is, complications arise during or after surgery. This is the case because everyone’s body is different. The composition of connective tissue varies widely from one patient to another, for instance, and this means that each patient’s healing process is entirely unique. This is why some people tend to develop thick scar tissue (known as keloid scar tissue) after any kind of penetrating skin injury, while others can sustain deep cuts and develop only subtle scarring that fades over time. Another good example of this difference is the way some women will develop severe stretch marks during pregnancy no matter what they do to prevent them, whereas other women emerge from pregnancy nearly stretch mark-free. Additionally, everyone’s immune system responds differently to stimuli. Just like some people have bodies that reject medical implants (despite the fact that these are designed to be completely biocompatible), some patients’ immune systems react poorly to implants inserted for cosmetic reasons.
Sometimes, no matter how skilled a patient’s plastic surgeon is, complications arise during or after surgery. This is the case because everyone’s body is different. The composition of connective tissue varies widely from one patient to another, for instance, and this means that each patient’s healing process is entirely unique. This is why some people tend to develop thick scar tissue (known as keloid scar tissue) after any kind of penetrating skin injury, while others can sustain deep cuts and develop only subtle scarring that fades over time. Another good example of this difference is the way some women will develop severe stretch marks during pregnancy no matter what they do to prevent them, whereas other women emerge from pregnancy nearly stretch mark-free. Additionally, everyone’s immune system responds differently to stimuli. Just like some people have bodies that reject medical implants (despite the fact that these are designed to be completely biocompatible), some patients’ immune systems react poorly to implants inserted for cosmetic reasons.